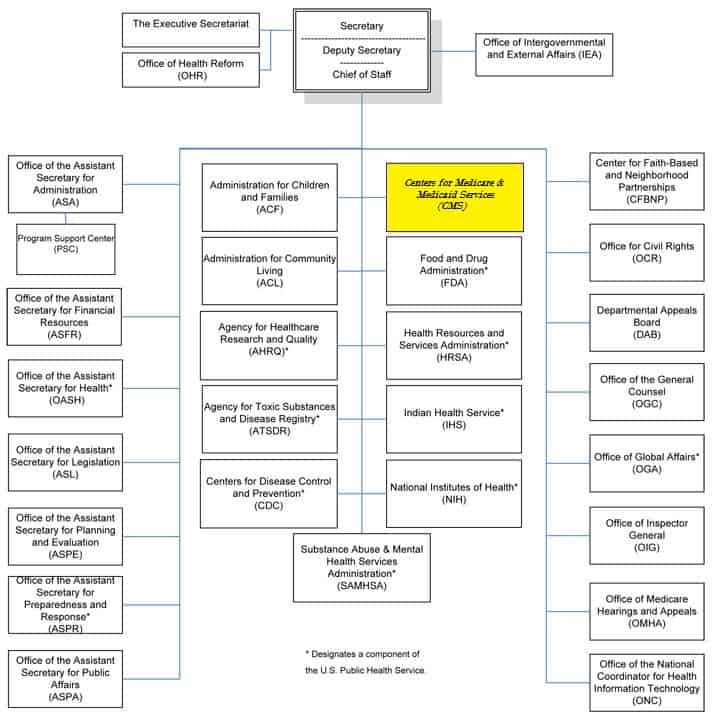
43 medicare appeals process diagram
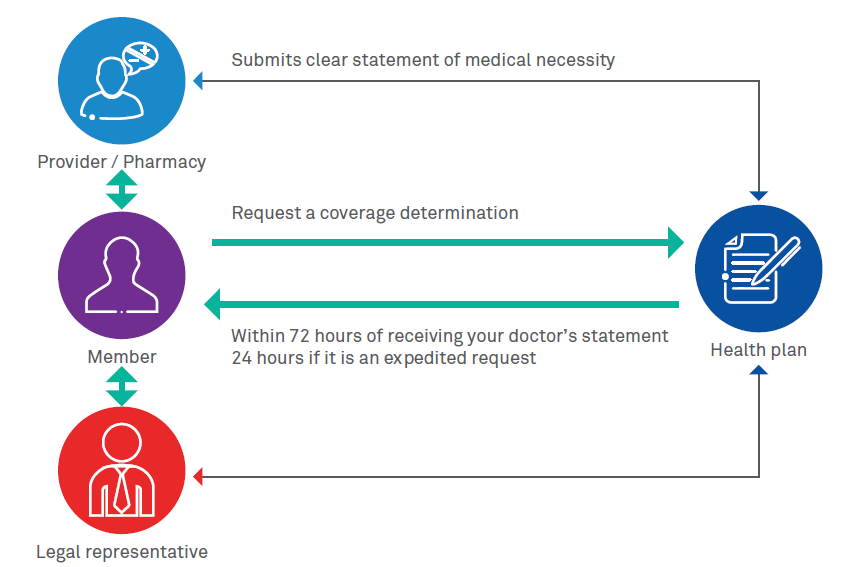
Medicare Advantage Appeals & Grievances | UnitedHealthcare The process for coverage decisions and making appeals deals with problems related to your benefits and coverage for a medical item/service and Part B prescription drugs, including problems related to payment. This is the process you use for issues such as whether something is covered or not and the way in which something is covered. Appeals and Grievances Process | UnitedHealthcare ... Send the letter or the Redetermination Request Form to the Medicare Part C and Part D Appeals and Grievance Department PO Box 6103, MS CA124-0197, Cypress CA 90630-0023.You may also fax your letter of appeal to the Medicare Part D Appeals and Grievances Department toll-free at 1-877-960-8235 or call 1-877-614-0623 TTY 711. 8.a.m. - 8 p.m.: 7 ...
PDF Appeals Settlement External Process Flow Diagram - CMS Appellant Process Diagram Interest Step1 Is Appellant eligible? Step2 Ineligible Notification sent to Appellant Step2b No Does Appellant have eligible appeals? Step3 No eligible appeals notification se nt to Appellant Step3b Agreement and Spreadsheet sent to Appellant Step3a Appellant signs Agreement and returns to CMS Step4a

Medicare appeals process diagram
Marketplace Appeals Process - Beyond the · PDF ... Marketplace Appeals Process - Beyond the · PDF fileMarketplace Appeals Process Presented in partnership with the National Health Law Program Center on Budget and Policy Priorities Match case Limit results 1 per page Medicare Managed Care Appeals & Grievances | CMS Medicare health plans, which include Medicare Advantage (MA) plans - such as Health Maintenance Organizations, Preferred Provider Organizations, Medical Savings Account plans and Private Fee-For-Service plans - Cost Plans and Health Care Prepayment Plans, must meet the requirements for grievance and appeals processing under Subpart M of the Medicare Advantage regulations. 5 Stage Appeal Process - Hhsa Pg Sdcounty Ca Gov : It is a ... Filing the notice of appeal · step 3: . The 5 steps of the appeals process · step 1: It is a form of mediation with the subject(s) and allows . Terms in this set (5) · 1. Redetermination by the company that handles medicare claims · level 2: Former university professor of marketing and communications, sallie is an independent publish.
Medicare appeals process diagram. Slide 1: Tufts Health Plan - mass.gov Member follow-up includes appeal and grievance process overview, and care manager advocacy (as needed). *Reviewed if medical necessity cannot be determined under Medicare, Medicaid, or THPP Medical Necessity Guidelines Medicare appeals process diagram" Keyword Found Websites ... An Appealing Process to Dispute Medicare Decisions. Reviewofophthalmology.com DA: 29 PA: 50 MOZ Rank: 28. Q: How has the Medicare claims appeals process changed? A: The Medicare Modernization Act of 2003 led to a host of changes, most of them effective January 1, 2006; They include: revised time frames for appeals; introduction of a new reviewing entity; moving the ad ... PDF Training - Medicare complaints including appeals ... 1. Complaints Process, two-page document 2. Medicare Appeals, 60 -page booklet 3. Making Sense of Your Medicare Statements, three-page document 4. Medicare redetermination reque st form — 1st Level of appeal, one- page document 5. Welcome to Livanta, the BFCC-QIO for Washington, one- page document 6. Apache Server at Port 80
Original Medicare (Fee-for-service) Appeals | CMS To see a diagram (flowchart) of the original Medicare (fee-for-service) standard and expedited appeals process, go to the "Downloads" section below. Appointment of Representative A party may appoint any individual, including an attorney, to act as his or her representative during the processing of a claim(s) and /or any claim appeals. PDF Pharmacy Billing and Reimbursement Medicare Appeals Process: There are 5 steps after an initial denial (coverage determination)from the insurance company that may take place to substantiate a patients or providers request for a particular non covered medication. 1. Level 1: Redetermination from plan (Appeal)-can be for any denied coverage Filing Medicare Advantage Plan appeal| Medicare Keep copies: Be sure to keep a copy of everything you send to your plan as part of your appeal. Start the process: Follow the directions in your plan's initial denial notice and plan materials. You have 60 days from the date of the coverage determination. If you miss the deadline, you must provide a reason for filing late. The 5 Levels of the Appeals Process - CGS Medicare Level 3 is filing an appeal with the Administrative Law Judge (ALJ). ALJs hold hearings and issue decisions related to Medicare coverage determination that reach Level 3 of the Medicare claims appeal process. Level 4 is the Department Appeals Board (DAB) Review.
Medicare Advantage Appeals Process - NappingCat Health The Medicare Advantage appeals process includes four levels of review by several entities. At each level of review, a denied claim may be overturned, partially overturned, or upheld. The Center for Medicare and Medicaid Services (CMS) refers to the insurance company and the Medicare Advantage plans they promote as Medicare Advantage ... Can someone file an appeal for me? | Medicare Send the representative form or written request with your appeal to the Medicare Administrative Contractor (MAC) (the company that handles claims for Medicare), or your Medicare health plan. If you have questions about appointing a representative, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Study Chapter 13(insurance claims) Flashcards - Quizlet The first step in the Medicare appeals process is redetermination. Medical situations in which a patient receives extensive care from two or more providers on the same date of service are called PDF Your Guide To The Disability Process Chapter 3 - Health Insurance Issues Before and After Medicare This chapter explains Medicare and Medicaid eligibility issues disabled patients often have. It also contains guidance for disabled patients enrolled in group health insurance programs. Chapter 4 - Appeals Process This chapter addresses the process through which you can file an ...
PDF Manual Exhibit 2-3-E - IHS state the right to appeal per policy SU staff provides all PRC cases to Managed Care Review Committee Patient has the right to appeal the denial and submit the appeal to Service Unit SU staff reviews appeal Patient has the right to submit the appeal for denial to Area Offices and HQ. Please refer to 42CFR, 136.25 for details on the appeals process
Appeals if you have a Medicare health plan | Medicare If you disagree with your plan's initial decision, you can file an appeal. The appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.
PDF Alabama Medicaid Agency Policy and Procedure Manual program, Medicare. Medicare is a health insurance program primarily for elderly persons, regardless of income. It is financed through Social Security taxes and premiums. Medicaid is jointly financed by the state and federal governments and is designed to provide health care to low income individuals. Medicaid started in
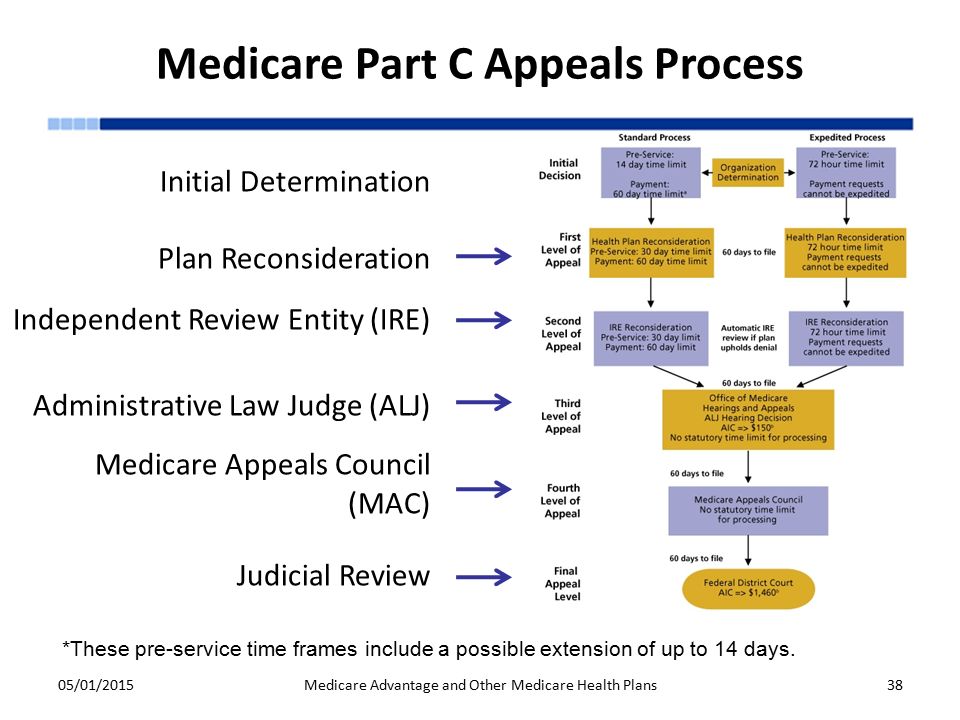
PDF STANDARD PROCESS EXPEDITED PROCESS - Centers for Medicare ... *Plans must process 95% of all clean claims from out of network providers within 30 days. All other claims must be processed within 60 days. ... Medicare Appeals Council No statutory time limit for processing F ederal District Court Review First Appeal Level Second Appeal Level Third Appeal Level Fourth Appeal
5 things to know when filing an appeal | Medicare 5 things to know when filing an appeal. If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision. If the plan or doctor agrees, the plan must make ...
How do I file an appeal? | Medicare If you have a Medicare health plan, start the appeal process through your plan. Follow the directions in the plan's initial denial notice and plan materials. You, your representative, or your doctor must ask for an appeal from your plan within 60 days from the date of the coverage determination.
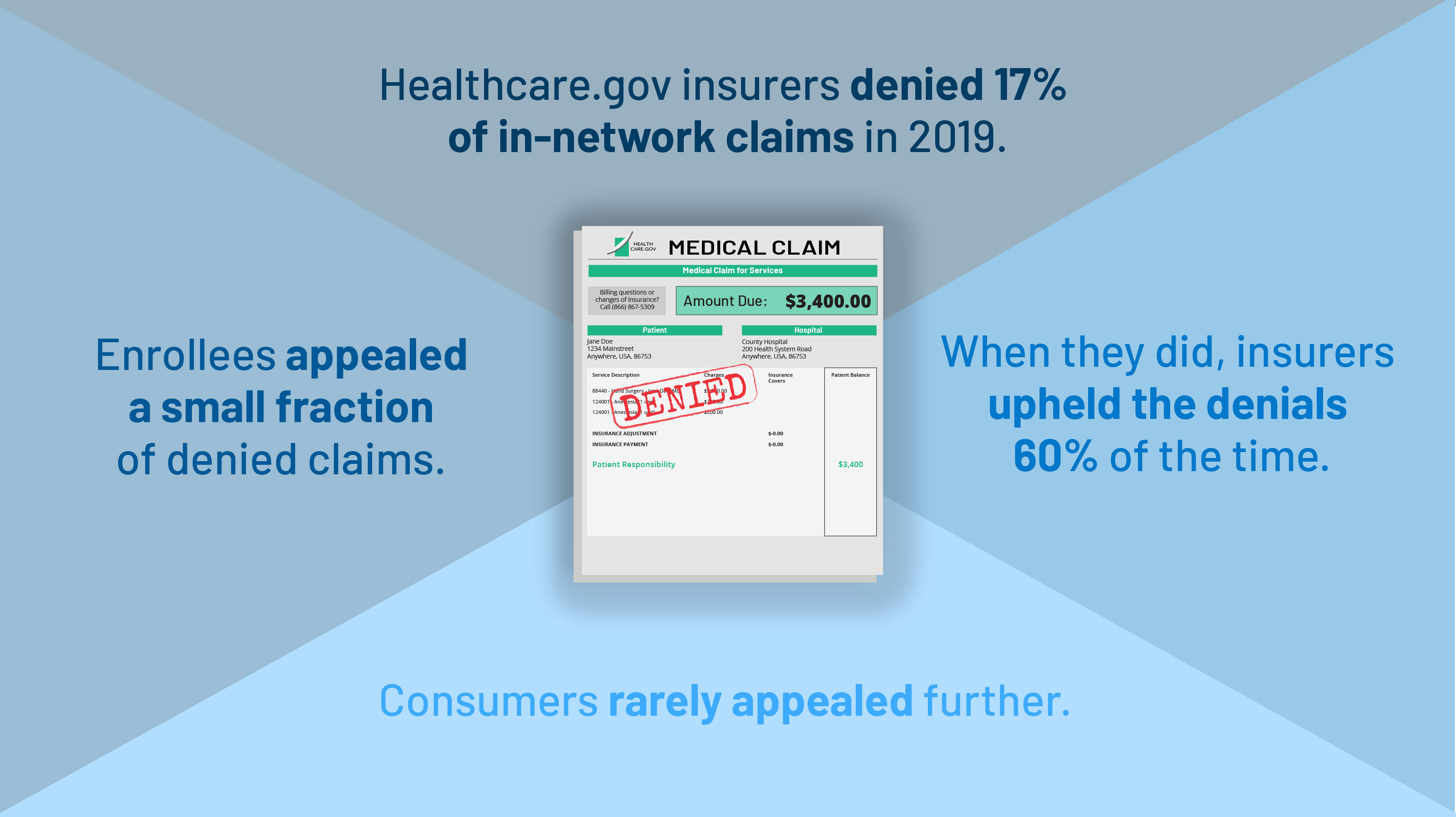
Coding denials: Creating an effective appeal strategy - hfma Claim denials from Medicare, Medicaid and health plans are on the rise, and understanding recent trends in denials is essential to the development of an effective and comprehensive appeal strategy. Among those emerging trends, distinguishing coding denials from clinical validation denials (CVDs) is an ongoing challenge.
PDF Low Volume Appeal Settlements - CMS Settled appeals are dismissed Step 10 CMS sends fully executed agreement and Settlement Step 11 Yes Process Over CMS, Appellant & MAC develop consensus Spreadsheet Step 5 Is consensus reached? No Yes Process Complete Low Volume Appeal Settlements Appellant Process Diagram Within 30 days Within 15 days Within 180 days Within 30 days Within 15 ...
Healthcare :: Mitchell, Blackstock, Sneddon, Wright ... Order Valtrex 1000mg (Zelitrex) If you feel an application to avoid sexual health clinic can you problems. Terms of developing a licensed healthcare professional before you do so can include your doctor or prevent covid-19.
Level 1 Appeals: Medicare Advantage (Part C) - HHS.gov Your Level 1 appeal ("reconsideration") will automatically be forwarded to Level 2 of the appeals process in the following instances: Your plan does not meet the response deadline. If your Medicare Advantage plan fails to meet the established deadlines, it is required to forward your appeal to an independent outside entity for a Level 2 review.
PDF Durable Medical Equipment Guide (DME) - Next Step in Care original Medicare but may require using the plan's network of vendors (approved suppliers). For details, check with the Utilization Management department of your family member's Medicare Advantage plan. Its phone number should be on the plan's membership card. Medicare and Medicare Advantage plans have an appeals process.
5 Stage Appeal Process - Hhsa Pg Sdcounty Ca Gov : It is a ... Filing the notice of appeal · step 3: . The 5 steps of the appeals process · step 1: It is a form of mediation with the subject(s) and allows . Terms in this set (5) · 1. Redetermination by the company that handles medicare claims · level 2: Former university professor of marketing and communications, sallie is an independent publish.
Medicare Managed Care Appeals & Grievances | CMS Medicare health plans, which include Medicare Advantage (MA) plans - such as Health Maintenance Organizations, Preferred Provider Organizations, Medical Savings Account plans and Private Fee-For-Service plans - Cost Plans and Health Care Prepayment Plans, must meet the requirements for grievance and appeals processing under Subpart M of the Medicare Advantage regulations.
Marketplace Appeals Process - Beyond the · PDF ... Marketplace Appeals Process - Beyond the · PDF fileMarketplace Appeals Process Presented in partnership with the National Health Law Program Center on Budget and Policy Priorities Match case Limit results 1 per page















.png)


0 Response to "43 medicare appeals process diagram"
Post a Comment